Population Health platforms are positioned as a strategy to address chronic illness with a primary focus on the clinical space. Powerful tools analyze registries of chronically ill patient data to improve outcomes. These platforms also serve as an early warning system for operational issues that need to be addressed by the healthcare system. The goal is to enhance the overall health of a specific patient population and maximize healthcare system performance.
I believe Population Health platforms are really targeted communication platforms. They communicate clinical information to doctors, operational data to health systems, and (attempt to communicate) relevant information to patients. The patient communication process represents an opportunity to enhance the power of these platforms.
How do you communicate?
In an earlier post I talked about three layers of a communication process: data, strategy and execution. All three layers need to work – or the communication process breaks down.
I included the following graphic in the post:
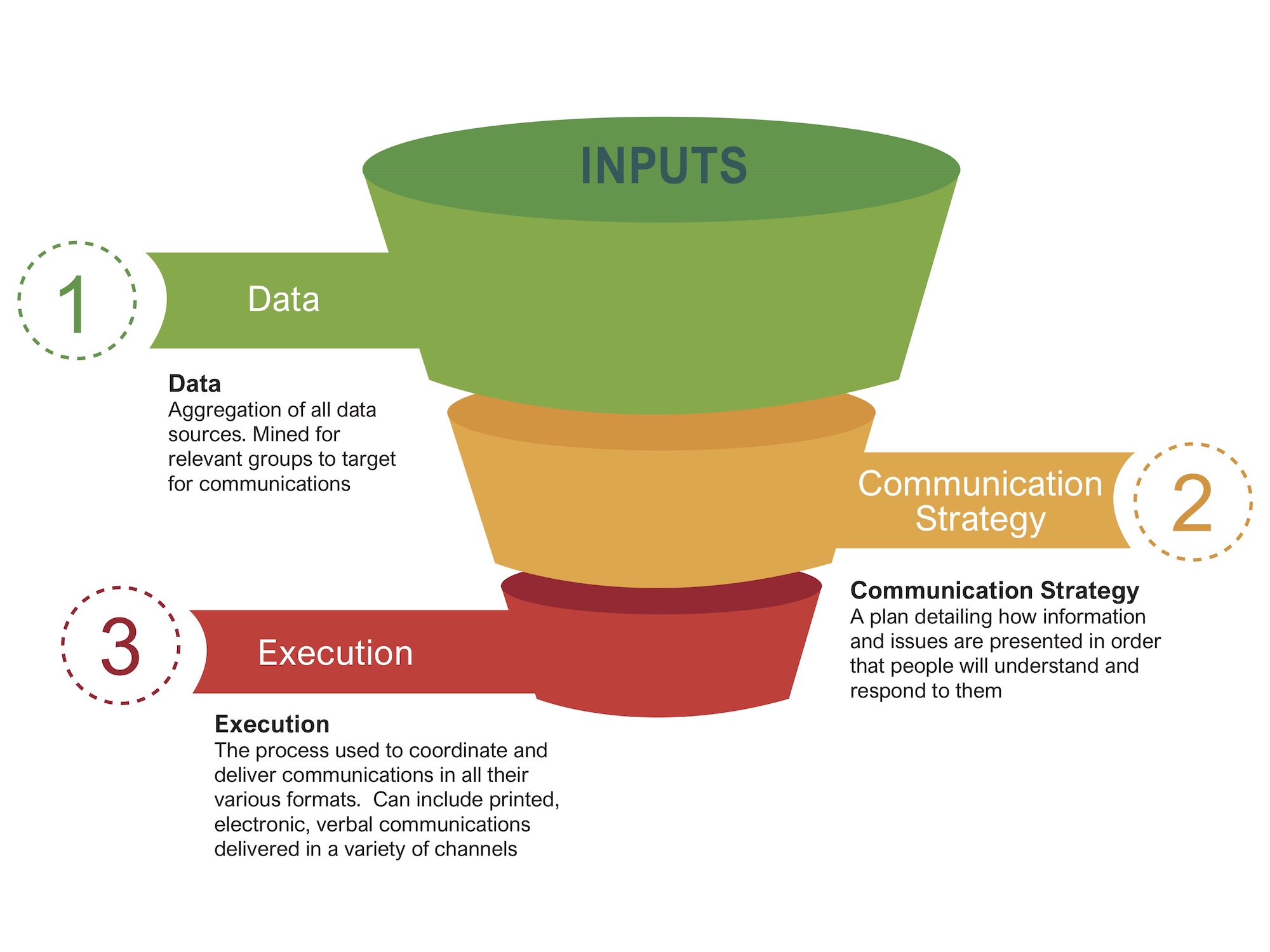
These three elements are straightforward:
- Data: Raw data forms the knowledge you have of your patients.
- Strategy: A plan on how to present information and issues to patients.
- Execution: The process used to coordinate and deliver the actual communications.
I created this graphic to describe the layers of a basic communication process. You could argue the layers are the same for a clinical approach to treatment. The physician gathers patient data, creates a treatment strategy and then executes the treatment.
Population Health as a clinical strategy
Population Health is viewed as a clinical strategy. What actions can a group of chronically ill patients take to maximize their health? Population Health also acts as an operational strategy for the healthcare system. What actions can a healthcare system take to improve target group outcomes and maximize reimbursements? This is an important element for healthcare systems. No debate there.
But Population Health platforms need to do more. They may start with a clinical/operational strategy, but they also need to manage the entire communications process to support ongoing treatment of chronically ill populations.
Why worry about communications?
The clinical data defining a specific chronic illness is fairly consistent. Likewise, the recommended treatment for chronically ill patient populations is fairly consistent.
The true variable right now in chronically ill populations is the patients — their language, education and culture which informs the way they interact with information and other people. What is the common thread in these patient variables? Communications.
Let’s take a look at the communication graphic changed for Population Health.

It’s still a communication strategy comprised of Data, Strategy and Execution, but with the focus on chronically ill populations:
- Population Health: The registry data available on a population with a specific chronic illness
- Health Communications: The use of health communication strategies to reduce barriers in language, education and culture which impact health literacy.
- Execution: The process used to coordinate and deliver the actual communications
Many current Population Health platforms are highly focused on using their power to gather and access data in order to help doctors with clinical activities and healthcare systems with operational management. The communication strategy seems more limited: patient/doctor interactions, varied communications describing a mostly standardized treatment and possibly some expensive care manager interactions.
How about some coordination?
The healthcare industry recognizes how fragmentation can impact outcomes. And are making efforts to reduce fragmentation of care. I have also posted about efforts to address data fragmentation.
How about communication fragmentation? Chronically ill patients interact with a variety of healthcare providers, each with their own communication strategy. Do they consistently communicate with chronically ill patients in their preferred languages and format? Is the treatment messaging consistent?
We need to add communication fragmentation to this discussion with a focus on two goals:
- Add a communication layer to the longitudinal patient record documenting patient communication preferences and language, education and culture. This will support consistent messaging across all touchpoints regardless of the originating healthcare provider.
- Standardize treatment messaging and imagery used by all providers who support and treat chronically ill populations as a way to coordinate and reinforce treatment goals.
Population Health platforms are best positioned to support these changes because, at their core, they are communication platforms for chronically ill populations. They focus on clinical treatment of patients that generate the greatest cost and provide information supporting clinical and operational efficiency. If they’re already attempting to address care fragmentation and data fragmentation, why not add communication fragmentation?
In future posts, I’ll discuss how research in cognitive science, computer science and graphic design might be used in messaging chronically ill populations in ways to improve health literacy while reducing barriers in language, education and culture.

No Comments