My last two posts talked about consumer and healthcare concepts of segmentation, data and interventions. I highlighted how consumer marketers focus heavily on response rates and Return on Investment (ROI). I also discussed the differences between the clinical and nonclinical space in healthcare regarding data access and movement.
Now let’s transition to a thought exercise which examines an ROI based approach to Social Determinants of Health (SDOH) interventions.
In some ways, it feels like a mismatch of capabilities. On the clinical side, there are powerful EHR and population health management capabilities healthcare systems use to segment, target, and track clinical care for chronically ill patients. Yet the symptoms used to diagnose these chronically ill patients – and the actual recommended interventions – are remarkably consistent.
The nonclinical side is more fragmented as SDOH capabilities in this space continue to be developed. They’re not nearly as fully built out as the clinical capabilities inherent in EHR and population health management systems. This is important because the growing body of research regarding determinants of health document the distinct aspects of patients’ lives affecting their ability to access and successfully utilize healthcare. And it highlights the real variability is not in the clinical diagnosis and treatment of chronic illness, but the nonclinical elements in every patient’s life – creating the potential for highly variable and expensive interventions.
I mentioned the possibility of treating nonclinical interventions like consumer marketing. In other words, building a system from the ground up to capture as much information as possible to generate customized interventions, gather feedback on the success of each element, and use powerful analytic tools to continually refine the approach to each individual patient.
The purpose of this post is to explore how we can move beyond our generic clinical focus on treating chronically ill patients to add on highly personalized nonclinical interventions to generate the greatest improvement in cost and outcomes across these patient populations.
What to do?
Many diverse groups are working on SDOH. Vendors are creating applications to identify local support organizations and their solutions can be connected to EHR systems to route patients to local, nonclinical support resources. There are also state waiver programs (like CalAIM in California) which seek to provide care management – and more – to people who are heavily impacted by social determinants of health. And why wouldn’t they? Affected by food or housing insecurity, transportation, and other nonclinical issues, large segments of our population access their healthcare through public insurance plans. Everyone is exploring ways to reduce overall cost.
But I need to highlight that, if our goal is to reduce cost, we need to examine the ROI for these interventions, especially in nonclinical areas because many will be expensive to implement. Offering transportation, healthy food, access to technology, and more requires not only a lot of coordination and management but a lot of money. If we adopt a more consumer marketing focused approach, we might consider the following actions:
First, create highly personalized nonclinical interventions that are relentlessly assessed for ROI. In other words, we target specific individuals with highly customized nonclinical interventions and follow up with deep analysis as to which elements generated the greatest reduction in overall cost and improved outcomes. Then reuse this knowledge to refine future interventions on a case-by-case basis.
Second, actively screen individuals for their impactibility (their propensity to react positively to the intervention). People exhibiting high levels of activation get increased SDOH support. Individuals with low levels of activation get basic SDOH support and educational campaigns seeking to improve their buy-in. As their activation improves, SDOH investment increases.
An Alternative Approach
Segmenting patients by cost is a good starting point with a focus on patients who generate high claims cost on a yearly basis. A healthsystemtracker.org article stated the following:
In 2019, 5% of the population accounted for nearly half of all health spending. The 5% of people with the highest health spending had an average of $61,000 in health expenditures annually; people with health spending in the top 1% have average spending of over $130,000 per year.
Let’s begin by segmenting patients by $25K increments starting with $50K as the base (i.e., $50K-$75K, $75K-$100K, $100K-$125K, and so on). Then factor in nonclinical elements:
- SDOH. Document the individual barriers they face that prevent them from accessing healthcare.
- Impactability. Which patients are most likely to respond positively to an intervention?
- Activation. Which of them have the knowledge and skills to effectively manage their health?
If you segment the patient by cost, document the SDOH barriers they face, and identify the patients who exhibit higher levels of impactability and activation, you can craft specific SDOH oriented interventions which vary by cost, targeted barriers and messaging.
At this point it becomes a discussion on results.
- Would you invest an average of 10% of an individual patients’ yearly claims cost in SDOH intervention if it resulted in a 20% reduction in clinical spend?
- For example, with a patient in the $100K per year category, would we spend $10K per year on SDOH barriers to get $20K in reduced claims cost (100% ROI)?
- Would you accept a zero percent ROI where the intervention costs the same as the claims reduction if it resulted in better outcomes and higher patient satisfaction?
Clearly, there are a lot of different, acceptable outcomes. And healthcare systems and states may create their own set of acceptable goals.
As you build institutional knowledge of how each element of intervention affects ROI, you might add a new measurement to risk stratification: segmenting patients based on their overall SDOH ROI in the form of reduced claims cost. Look at the following chart:
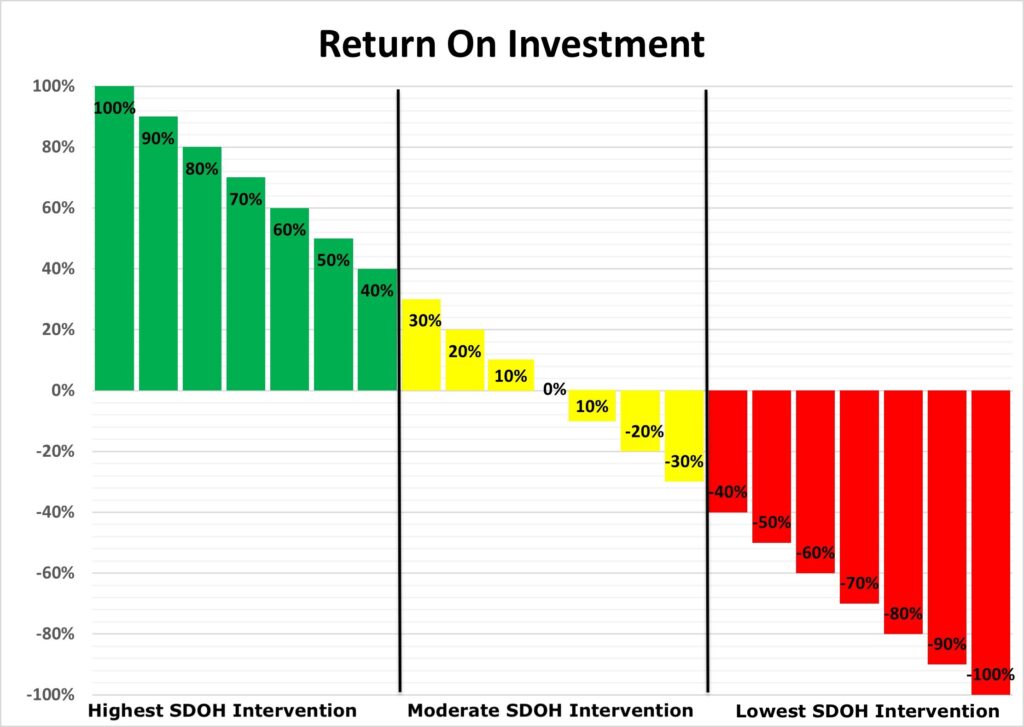
For patients represented in green (40% or greater ROI), you commit the greatest SDOH investment. For patients represented in yellow (30% to -30% ROI), you offer a moderate SDOH investment with education. For patients represented in red (-40% or lower ROI), you offer basic SDOH investment with a higher focus on education to improve their health literacy.
Keep in mind this is an example of how these future decisions might be determined, because any nonclinical interventions will be publicly funded. Can we afford to spend the same on everyone, including patients who demonstrate a complete lack of engagement? Maybe our future involves prioritizing patients who generate the greatest savings (ROI) to maximize overall cost reductions? If you maximize savings by targeting the highest ROI identified patients, you can repurpose those savings towards programs designed to improve low ROI patient participation.
At the end of the day, we want to improve the conditions of as many chronically ill patients as possible. But if we also want to reduce the incredible healthcare spend in our country, we may have to consider putting a priority on the patients who represent the greatest ROI for these potentially costly interventions.
Longer term
Healthcare systems have so much on their plate right now, I doubt they’d take the lead on this. I suspect our federal or state governments would have to fund pilot programs to evaluate the ROI of a variety of customized interventions based on the metrics defined above. They would have to partner with a strong Population Health vendor (and a strong healthcare system) to identify participating patients, create sufficient network density to accurately capture participation and savings data, then develop the population health platform tools to calculate ROI and identify the intervention elements that generated the greatest positive impact.
Who knows? Over the next few years, we may develop the application and data gathering capabilities to offer highly personalized SDOH oriented support that transforms the lives of at-risk patient populations, while maximizing overall claims cost savings and outcomes.
In my next post, I’ll examine patient engagement in low adherence patients.


No Comments