In my previous post, I wrote about technology and services implementations and how our government incents healthcare providers through payment models that provide incentives for lower costs and better outcomes. One point I emphasized was these inducements will likely become more stringent over time. The current cost of treating chronically ill patients is far too great and our government will continue to ratchet up pressure to generate change.
Recently, I found a 2021 report by the National Academy of Sciences, Engineering and Medicine called Implementing High Quality Primary Care: Rebuilding the Foundation of Health Care. You can read and download the entire report at this link.
I found this report fascinating on several levels. The authors made a wide variety of recommendations. First and foremost, primary care doctors should be positioned as the most important element of reimagined healthcare. Second, primary care should be available to everyone. Third, we should consider capitated primary care, so physicians have the time they need to understand the whole patient – not only their illness, but their entire life including family and community. Only then will we transform healthcare.
The study also highlighted several issues with our current healthcare structure and all of them apply to chronically ill populations, especially in lower income households. Many such households have high deductible health plans, forcing the patient to cover 100% of all primary care until their deductible is met. As a result, many patients don’t go to the doctor until they’re truly ill, generating far higher expense via specialist care and hospitalizations.
There’s too much to cover in a blog post, but I want to highlight a few areas that point to the need for better communication.
Communication is key!
The summary of the study contains a key section:
High-quality primary care is the foundation of a high-functioning health care system and is critical for achieving health care’s quadruple aim (enhancing patient experience, improving population health, reducing costs, and improving the health care team experience). High-quality primary care provides comprehensive person-centered, relationship-based care that considers the needs and preferences of individuals, families, and communities.
The last sentence goes beyond the clinical focus to accommodate the needs and preferences of the patient, families, and community. This is an important point. In my first post on this blog, I highlighted a slide deck published by the CDC that focused on improving medication adherence in chronically ill patient populations. One of the CDC slides (see below) highlighted the value of bi-directional communication, which is a key element of person-centered, relationship-based care.
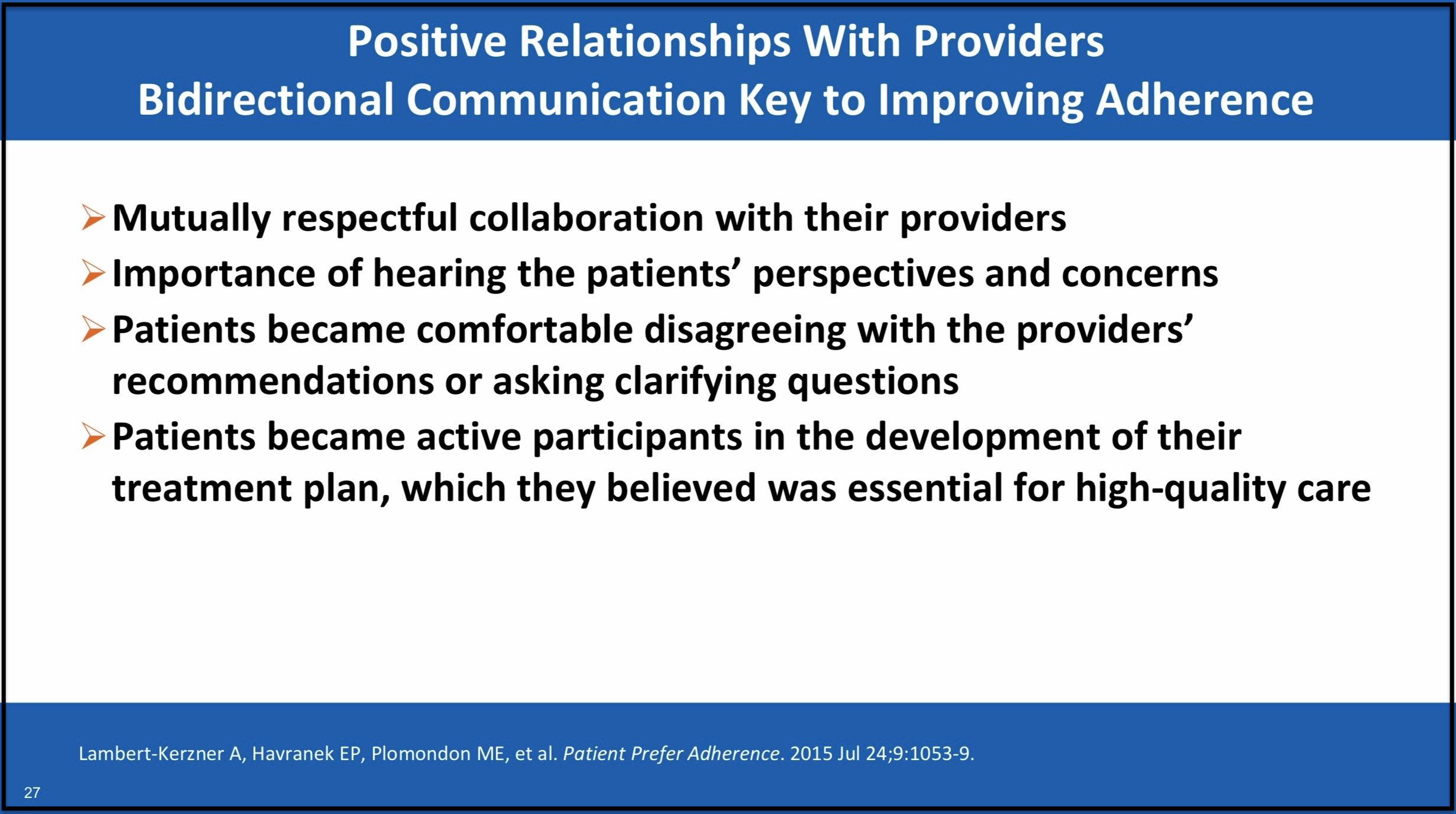
Each of the points on this CDC published slide highlight how patients do want care that comprehends their perspectives and concerns. You can download the entire deck of slides here.
Non-clinical information is critical
The National Academy study also highlights five objectives for reimagining primary care with corresponding actions under each. Some are structural and others are financially focused.
- Pay for primary care teams to care for people, not doctors to deliver services.
- Ensure that high-quality primary care is available to every individual and family in every community.
- Train primary care teams where people live and work.
- Design information technology that serves the patient, family, and interprofessional care team.
- Ensure that high-quality primary care is implemented in the United States.
The first three objectives are straightforward. Allocate more money to primary care, so physicians can step off the fee for service treadmill. Make primary care available to all, then place resources where people live and work. The fifth is the hammer that makes it happen.
The fourth bullet (in bold) is the one that caught my eye, and it has an action underneath it that states the following:
Action 4.1.A: Align with the functions of primary care—supporting the relationship between clinicians, care teams and patients; providing access and continuous contact over time; collecting and understanding the patient’s story; and focusing on the patient and family rather than the disease.
The last italicized and bolded section (my emphasis) represents a deeper explanation of person-centered, relationship-based care. This flips the focus from the clinical (the actual disease) to the non-clinical (patient story, patient and family). To do this, the study recommends incenting primary care physicians to spend as much time as possible with patients, so they can truly understand their story. We pay more for primary care which reduces the reliance and incidence of specialist care and hospitalizations. Overall, we reduce healthcare spend and improve the quality of life for all patients.
Even more, the study recommends a hybrid approach to healthcare insurance with a mix of capitated and fee for service payments. More of the capitated payment would be focused on a primary care team – and fee for service payments would be reduced in some fashion. The goal is to create a true medical home where both clinical and non-clinical information are gathered, stored, and used to keep patients healthier. The study believes this is an achievable step within our current healthcare insurance ecosystem. Frankly, I wouldn’t be surprised if our government proposes some form of this for chronically ill patient populations.
Worth a look
This study contains a lot of information and I recommend downloading it to review. There is a long list of recommendations that would require transformational change in how we approach healthcare. Unfortunately, many of them would find resistance from the entrenched partisan interests which currently exist in our healthcare system. For example, the study highlights how primary care and specialty care generate roughly the same number of patient visits each year, but specialty care bills over three times the revenue of primary care. You can easily imagine how they might want to protect that revenue stream.
I personally found the study interesting because it elevates the importance of two key areas I’ve talked about repeatedly on this blog.
- Data on patient non-clinical preferences and socioeconomic status is critical to future healthcare success.
- The use of two-way communication to understand all facets of the patient’s life, and how it contributes to their current healthcare issues, is required.
We should keep our current focus on payment models that incent providers to reduce cost and generate better outcomes. But as I’ve mentioned in several of my previous posts, this approach will only take you so far. There is only so much efficiency you can capture in clinical operations. Real change will come from reducing usage via improved health literacy. This study’s recommendations of reimagining primary care to encompass the entire clinical and non-clinical life of patients, and emphasizing highly personalized communications, seems like a winner.


No Comments